Understanding Its Causes, Recognising the Symptoms, and Exploring Treatment Options and Prevention Strategies
 What Is Denture Stomatitis?
What Is Denture Stomatitis?
At Tracey Bell Dental and Aesthetic Medical Clinics, we often encounter patients experiencing discomfort from their dentures, not realising it might be denture stomatitis. This condition, characterized by inflammation of the mouth’s mucous membrane beneath the denture, is more common than many think. While it might sound alarming, understanding its nature is the first step towards treatment.
The Aetiology: What Causes Denture Stomatitis?
Denture stomatitis primarily arises from the overgrowth of Candida yeast, a fungus that ordinarily lives in the mouth’s ecosystem without issue. However, certain conditions, such as poor dental hygiene, continuous wearing of dentures, or an improper fit, can create an environment where this yeast thrives, leading to inflammation.
Factors contributing to this imbalance include:
- Poor Oral Hygiene: Neglecting the cleanliness of both the dentures and the mouth can encourage fungal growth.
- Continuous Wear: Wearing dentures without breaks, especially at night, deprives the mucosal surface underneath of necessary exposure to air and saliva, which have natural antimicrobial properties.
- Ill-Fitting Dentures: Dentures that don’t fit correctly can create pressure points and restrict blood flow, weakening the mouth’s natural defences against infection.
Understanding these causes helps us tailor a prevention and treatment strategy that’s both effective and manageable.

Recognising the Signs and Symptoms
Denture stomatitis can manifest in several ways, and being vigilant about symptoms is key to early detection and treatment. Symptoms to watch for include:
- Redness and Swelling: The most common sign, often noticed beneath the denture.
- Sore Spots: These can occur where the denture rubs or presses excessively.
- Burning Sensation or Dryness: Many patients report a burning sensation, particularly common in the morning, or an unusual dryness.
- Bad Breath or Taste: An overgrowth of Candida can cause a distinct bad taste or breath.
Early recognition of these symptoms allows for quicker consultation and treatment, significantly improving outcomes.
The Treatment Pathway
 Initial Steps
Initial Steps
Improving denture hygiene is often the first and most crucial step. This includes:
- Daily Cleaning: Dentures should be cleaned daily with a soft brush and non-abrasive cleaner specifically designed for dentures.
- Proper Rinsing: After meals, removing and rinsing dentures can help remove food particles and reduce the risk of irritation.
Medical Treatments
When hygiene improvements aren’t sufficient, we may recommend antifungal medications. These are effective at reducing Candida levels and are available in various forms to suit different needs and preferences.
Addressing Underlying Issues
Addressing ill-fitting dentures can alleviate much of the discomfort and risk associated with denture stomatitis for many patients. Our clinic specializes in assessing and adjusting dentures for the perfect fit, ensuring they provide support without causing unnecessary pressure or irritation.
Prevention Strategies
Preventing denture stomatitis involves a comprehensive approach to oral hygiene and denture care. Key strategies include:
- Nightly Removal: Allowing gums to rest and recover overnight is crucial.
- Regular Dental Check-ups: These enable early detection and treatment of potential issues.
- Proper Denture Care: Including regular cleaning and maintenance of dentures.
Treatment Pathway Enhanced: Recommended Drugs
While improving hygiene practices forms the bedrock of managing denture stomatitis, there are cases where medication becomes necessary. It’s crucial to follow a treatment plan based on current, evidence-based guidelines, such as those provided by the SDCEP.
 Local Measures
Local Measures
The first line of defence against denture stomatitis involves local measures. These include:
- Daily Brushing of the Palate: This simple step can significantly reduce irritation and inflammation.
- Thorough Denture Cleaning: Soaking dentures in chlorhexidine mouthwash or sodium hypochlorite for 15 minutes twice daily is recommended. However, due to its bleaching properties, sodium hypochlorite should only be used for acrylic dentures.
- Reducing Denture Wear: Patients should be encouraged to leave their dentures out as much as possible during the treatment period to allow the underlying tissues to recover.
Should the dentures contribute to the issue, adjustments or the creation of new dentures may be necessary to prevent recurrence.
 Pharmacological Interventions
Pharmacological Interventions
When local measures are insufficient, pharmacological treatment may be advised. It’s essential to consider the patient’s overall medication profile due to potential drug interactions, especially with medications like warfarin and statins.
Fluconazole
Fluconazole is a common choice, with a typical 7-day regimen being:
- For Adults: 50 mg capsules, one capsule daily.
- For Children: Dosing varies by age, with a maximum of 50 mg daily for older children and a weight-based dose for younger ones.
Due to its interactions, fluconazole should not be prescribed to patients taking certain medications, including warfarin and statins. Its use for treating denture stomatitis is limited to a maximum of 14 days.
Miconazole
Miconazole, available as an oromucosal gel, is another option:
- For Adults and Children Over 2 Years: Apply a pea-sized amount to the fitting surface of the upper denture four times daily after food.
Patients are advised to continue use for 7 days post-healing. Miconazole’s absorption means it should also be avoided in patients taking warfarin or statins.
Nystatin
Nystatin serves as an alternative if fluconazole and miconazole are contraindicated, with a 7-day regimen of oral suspension administered four times daily after meals. Patients should remove their dentures before using the drug and continue use for 48 hours after lesion healing.
Conclusion
While common, denture stomatitis is highly treatable and often preventable with the right care. At Tracey Bell Dental and Aesthetic Medical Clinics, we are dedicated to ensuring our patients not only enjoy a beautiful smile but also maintain the health and comfort of their mouths. By understanding the causes, recognising the symptoms early, and following a tailored treatment and prevention plan, we can effectively manage denture stomatitis, ensuring you continue living with confidence and comfort.
Managing denture stomatitis effectively involves a combination of improved hygiene practices and, where necessary, pharmacological treatment guided by the latest evidence-based recommendations. At Tracey Bell Dental and Aesthetic Medical Clinics, we are dedicated to providing our patients with the highest standard of care, guided by the latest clinical evidence and guidelines, such as those offered by SDCEP. Our approach ensures that each patient receives personalised, effective treatment and advice, helping them overcome denture stomatitis and maintain optimal oral health.
Remember, the information provided here, especially regarding medication, is based on guidelines as of BNF 85 (March 2023) and BNFC 2022-2023. Always consult a healthcare professional for the most current treatment options suitable for your circumstances.
A Case Study – NO teeth but Pain
A Reflection on Transforming Oral Health: A Patient’s Path to Healing
Introduction
Six weeks ago, a story unfolded in our clinic that deeply reminded me of why I chose dentistry as my profession. A 72-year-old lady came to me in despair, suffering from severe oral pain that no absence of natural teeth could alleviate. The corners of her mouth cracked painfully, a constant discomfort that mirrored the state of her oral health. Upon examining her dentures, which had been her companions for over 15 years, the diagnosis was unmistakable: denture stomatitis. This case study embodies the profound change that education, straightforward dental interventions, and appropriate medical treatment can bring to a person’s life.
The Story Begins
She told me, with a mix of resignation and hope, that her mouth had been a source of constant pain for 3 to 4 years. Despite seeking help, the root of her discomfort remained unnamed. Her confession that she had never been taught how to care for her dentures struck a chord with me. Her cleaning routine was rudimentary at best, limited to soaking them in salt water without using a toothbrush. Concerns about the cost and comfort had deterred her from considering new dentures. Realising the extent of her need, we proposed a treatment plan that was what she could afford and effective:
- A Lesson in Denture Hygiene: She stresses the critical importance of brushing her dentures and the necessity of cleaning the fitting surface to combat plaque and fungal growth.
- Making Adjustments: To alleviate her concerns about comfort and fit, we realigned her denture with a soft lining, ensuring it sat comfortably yet securely against her gums.
- A Nightly Routine: We encouraged her to remove her dentures at night, allowing her gums to rest and heal, minimising the moist environment in which fungi thrive in. Long term she would be able to sleep in them.
- Fighting the Fungus: Miconazole was the chosen medication used against Candida She applied it as instructed, showing commitment to recovery and self-care.
Within just six weeks, the pain had gone.
The pain that had been her constant companion for years had vanished.
At Tracey Bell Dental and Aesthetic Medical Clinics, we are dedicated to empowering our patients with knowledge and providing care that addresses not just the symptoms but the root of the problem. This person’s journey from enduring pain to being able to eat and smile has been a powerful reminder of the impact we can have.
Recognising and treating simple conditions like denture stomatitis can have a profound effect on patients as this simple treatment and care did.
Back to blog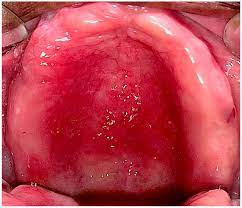 What Is Denture Stomatitis?
What Is Denture Stomatitis? Initial Steps
Initial Steps Local Measures
Local Measures Pharmacological Interventions
Pharmacological Interventions